Humana is deeply committed to the Medicaid program, recognizing its importance in providing quality health care to underserved populations. We focus on whole-person care that ensures our members have access to the resources they need to stay healthy.
Medicaid provides healthcare coverage for 70.5 million Americans.1 Coverage is open to people who meet income guidelines, including qualified families and children, pregnant women, seniors, and people with disabilities. Often, Medicaid benefits are free or low cost to those who qualify. The Medicaid program is administered by state governments within federal guidelines.
Most state Medicaid agencies choose to partner with private managed care companies, like Humana, to improve quality, outcomes, and enrollee experience. Managed care organizations enhance preventive care that makes Medicaid more cost-efficient. For example, Humana engages pregnant enrollees in maternity care programs that improve prenatal care and reduce avoidable preterm births and NICU stays. CMS defines minimum standards for eligibility and benefits, then each state has some flexibility to expand coverage.
Humana’s Medicaid Program
Humana’s Medicaid program manages complex populations and delivers innovative solutions to improve outcomes and enhance quality of life for the most vulnerable members of the communities we serve. With three decades of experience serving people with Medicaid, we have a wide range of capabilities and demonstrated success in integrating physical health, behavioral health, pharmacy, long-term care and social services. Together, these provide a whole-person approach to improve the health and well-being of our members.
In addition to clinical and care management programs, Humana’s Medicaid programs invest in community organizations that serve members locally and address their most urgent wellbeing needs. Through these partnerships, Humana helps meet the needs of families and communities in multiple ways, including maternal health, substance use disorder recovery, job training, food and housing insecurity, and more.
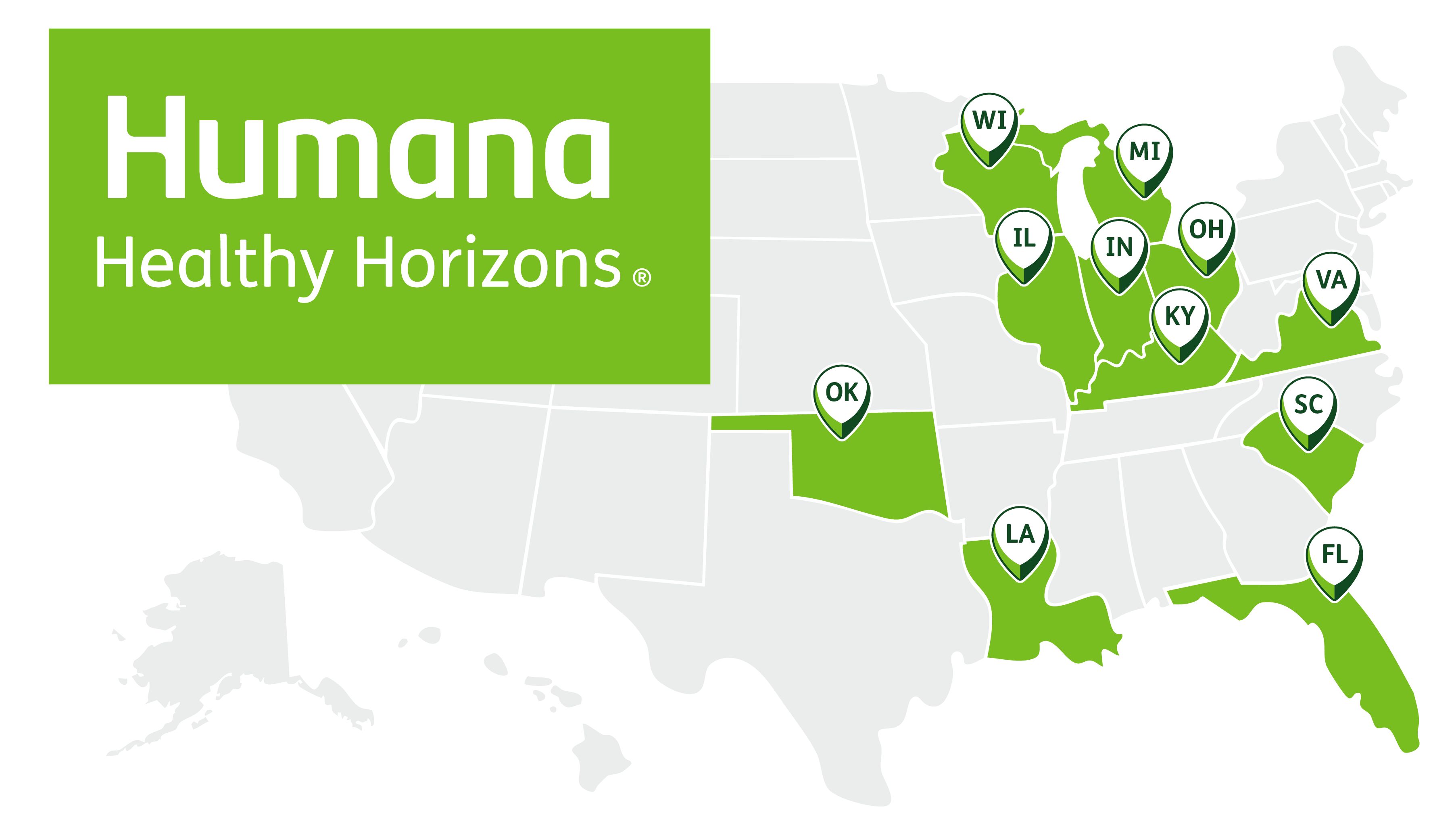
Currently, Humana's Medicaid program serves over 1.54 million Medicaid members across 11 states (Florida, Illinois, Indiana, Kentucky, Louisiana, Michigan, Ohio, Oklahoma, South Carolina, Virginia, and Wisconsin).2
1 CMS June 2025: Medicaid and CHIP Eligibility Operations and Enrollment Snapshot
Humana Medicaid Plans are available in 11 states
Extending our value-based care expertise to Medicaid
Humana’s longstanding experience in